The Stress-Resiliency of Our Body:
From the Stability of Our Internal Environment, Homeostasis to the Integrative Discovery of Hans Selye About Biologic Stress
By Oksana Zayachkivska, MD, PhD, DSc and Sandor Szabo, MD, PhD. MPH, DSc (h.c.)
Professors, School of Medicine, American University of Health Sciences, Signal Hill, CA
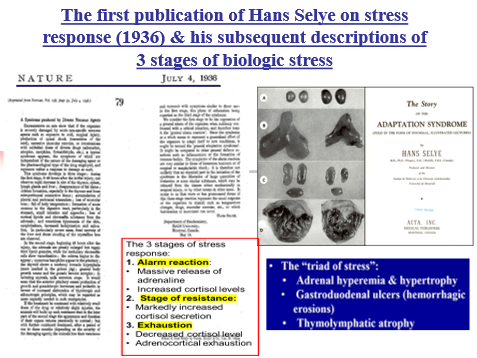
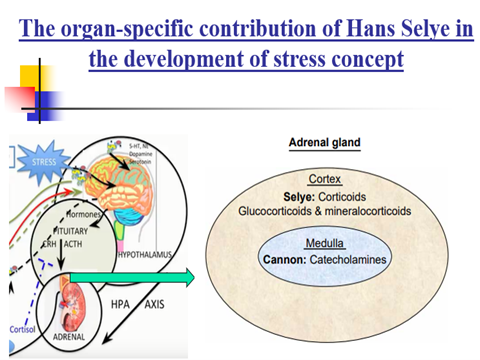
We were the course directors of the 10th International Summer School on Stress: Stress Education, Management & Resilience Training (SEMART), hosted by VIGS (Vienna Institute for Global Studies), Vienna, June 2-6, 2025. Here we want to summarize our introductory presentations and emphasize the historical discoveries about the stability of the body. Namely, the famous French physiologist Claude Benard ( Claude Bernard biography ) recognized in the middle of 19th century that despite outside variations of temperature, humidity, etc., our internal body temperature and chemical composition are remarkably stable. The American physiologist Walter Cannon ( Walter Cannon ) investigated this further in the first part of the 20th century & named this stability “homeostasis.” He is also famous for describing the “fight-or-flight” syndrome that he linked to the massive release of catecholamines, especially epinephrine/adrenaline from the medulla of the adrenal glands. These neurotransmitters are rapidly degraded in our body and remain effective only for a few minutes. Hans Selye (Nature, 1936, 1950) recognized the seminal role of the adrenal cortex from which glucocorticoids are released during the alarm reaction during this “general adaptation syndrome” that he later named the stress response. As opposed to the short-lived catecholamines, the steroid hormones remain active in our body for 3-4 hrs and are responsible for the morphologic triad of stress response.
Hans Selye’s concept of “cross-resistance ” describes how our bodies don’t just return to baseline after stress but can achieve improved states of adaptation. Later it transformed to stress resilience. It explains why people who navigate challenges skillfully often emerge stronger than they were before distress occurred. Physiological resilience is a term used to describe an individual’s capacity to mobilize the body’s adaptive potential regarding stress thresholds. Among various factors that shape its state are age, pre-existing health conditions, metabolic status, lifestyle choices, physical activity, sleep quality, nutrition, and acclimatization to cold or heat exposure.
High physiological resilience elevates the threshold at which stressors cause discomfort and harm, while low resilience increases vulnerability to identical stressors. Since personal metabolic status is crucial for developing physiological resilience, its predictive determinants can be used for understanding body’s stress resilience.

Every individual has a unique ” Stress resilience signature” which refers how body responds to and recovers from different types of stressors. This signature includes:
Autonomic Responsiveness: How quickly and intensely the sympathetic nervous system activates, and how efficiently the parasympathetic system initiates recovery.
Hormonal Patterns: Your cortisol rhythm, insulin sensitivity, and thyroid function all influence how you process stress and build resilience.
Metabolic Flexibility: Your ability to switch between different energy sources and maintain stable blood sugar under varying metabolic demands: postprandial (after meal) based on insulin, glucagon, incretin hormones (GLP-1, GIP), gastrin, adrenaline/epinephrine, leptin, ghrelin, circadian (e.g., growth hormone or melatonin), or ultradian (e.g. glucocorticoids) or diurnal rhythms (e.g. uncoupling protein 1 (UCP1) from brown fat).
Inflammatory Response: How your immune system reacts to stressors and how quickly inflammation resolves.
Understanding body’s physiological resilience allows you to design personalized protocols which will help to keep metabolic health. The “Three Pillars of Physiological Resilience” include:
Pillar 1: Responsive Activation – capacity to mount an appropriate stress response when challenges arise. This involves optimal functioning of your hypothalamic-pituitary-adrenal (HPA) axis, sympathetic nervous system, and metabolic systems.
Pillar 2: Efficient Recovery – our ability to baseline and initiate repair processes after stress exposure. This depends heavily on parasympathetic function, sleep quality, and nutritional status.
Pillar 3: Adaptive Growth – the capacity to use stress exposure to build greater future capacity. This involves neuroplasticity, metabolic flexibility, and the development of what Selye called “cross-resistance.”
This concept of physiological resilience as an integrative system of mobilization adaptive potential represents a promising target for addressing metabolic alterations, helps to understand modern view on different subtypes of obesity and its comorbidities. Interesting Danish research about increased brown fat deposits even in a sub-Arctic climate supports the notion that Selye’s words, “stress can make you stronger,” can be applicable to understanding contribution of physiological resilience on metabolic health by the brown-white fat dynamic.
In summary – although the stability of body started to be understood in middle of 19th century and it was expanded by the recognition of “fight-or-flight” syndrome linked to the massive release of short half-life catecholamines (epinephrine, norepinephrine). Subsequently, Hans Selye established the foundation of more complex adaptation syndrome (later named biologic stress) since it included the crucial role of corticosteroid hormones released from the adrenal cortex. He later recognized that short exposure to distress made the body more resistant to severe distress. This “cross resistance” led to the modern concepts of stress resilience.
References
- Selye H. A syndrome produced by diverse nocuous agents. Nature. 1936 Jul 4;138(3479):32. Available from: https://www.nature.com/articles/138032a0
- Selye H. The physiology and pathology of exposure to stress, a treatise based on the concepts of the general-adaptation syndrome and the diseases of adaptation. Montreal: ACTA, Inc., Medical Publishers. 1950.
- Szabo S, Tache Y, Somogyi A. The legacy of Hans Selye and the origins of stress research: a retrospective 75 years after his landmark brief “letter” to the editor# of nature. Stress. 2012 Jul 30;15(5):472-8. DOI: https://doi.org/10.3109/10253890.2012.710919
- Cabot, L., Erlenbeck-Dinkelmann, J., & Fenselau, H. Neural gut-to-brain communication for postprandial control of satiation and glucose metabolism. J. Endocrinol., 2023 258(3), e220320. https://doi.org/10.1530/JOE-22-0320
- Cypess AM. Reassessing human adipose tissue. N. Engl. J. Med., 2022 Feb 24;386(8):768-79.
- Zayachkivska O. Where is the place of the modern understanding of obesity in GI problems in Parkinson disease? Reviewing traditional models through contemporary view. J. Clin. Gastroenterol., 2025 July; 59(6): p 582.
- Motzfeldt Jensen M, Jørgensen MG, Elberling Almasi C, Andersen S. Effect of habitual cold exposure on brown adipose tissue activity in Arctic adults: A systematic review. Intern. J. Circumpolar Health. 2025 Dec 31;84(1):2545059.